Research Update: Platelet-Rich Plasma (PRP) Treatment for Chronic Tennis Elbow
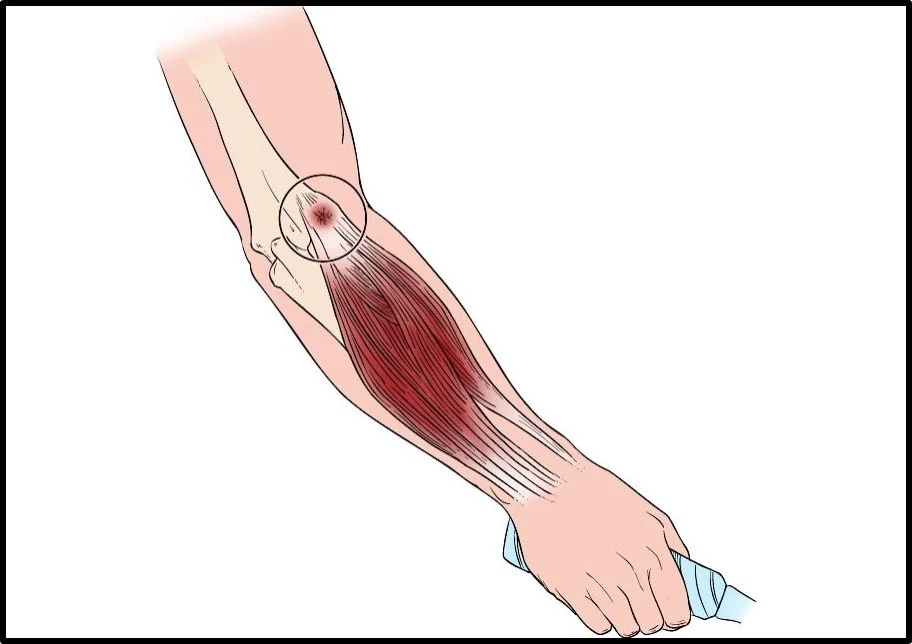
Reproduced and modified from The Body Almanac. © American Academy of Orthopaedic Surgeons, 2003.
What is Tennis Elbow?
The term “tennis elbow” is somewhat of a misnomer as most patients who experience the condition do not play tennis. Once thought to be a condition of inflammation on the lateral (outside) part of the elbow, new research has shown the condition is a chronic degenerative change within the common extensor tendon and may also include partial tears (Khan et al., BMJ, 2002; Kraushaar et al., JBJS, 2002; Rees et al., Rheumatology, 2006). The chronic structural damage to the tendon results in pain, decreased grip strength, and functional limitations which can impair manual work and athletic activity.
Tennis elbow effects 1-4% of the general population each year and up to 29.3% of laborers (Shiri et al., Best Pract Res Clin Rheumatol, 2011). Symptoms can linger for several months and at least one study has shown patients with greater than 6 months of symptoms often need surgical intervention (Sanders et al., Sports Health, 2016).
The Case Against Cortisone Injections
Cortisone injections were previously thought to be viable treatment options for tennis elbow. However, recent studies show cortisone injections may be harmful to tendons. Specifically, a recent systematic review of 16 basic science studies showed cortisone may decrease tenocyte (tendon cell) viability and function while also weakening the structure of the tendon (Puzzitiello et al., Arthrosc Sport Med Rehabil, 2020).
Alternative Solutions for Tennis Elbow
Given the prevalence of tennis elbow and acknowledgement that cortisone injections may actually harm the tendon long-term, interest has emerged in other non-surgical treatments to see if a more sustainable solution may exist.
A recent prospective randomized controlled trial evaluated multiple treatment options with outcomes reported up to 2 years after treatment (Lhee et al., Am J Sports Med, 2025).
Purpose of Study:
To evaluate whether PRP, prolotherapy, and shockwave therapy (ESWT) provide superior clinical outcomes over 24 months compared to physical therapy for patients with common extensor tendinosis (tennis elbow).
Courtesy of Allan K. Mishra, MD, Menlo Park, CA.
Key Study Methodology:
Patients older than 35 years with lateral elbow pain lasting more than 6 months were included
Diagnosis was made based upon physical examination and musculoskeletal ultrasound
Patients had failed at least 3 months of non-surgical treatment
Outcomes Measured:
DASH (Disabilities of the Arm, Shoulder, and Hand) Score – assesses arm function
SSS (Subjective Satisfaction Score) – measures patient satisfaction with treatment
Patients Enrolled:
202 patients completed the study and were evaluated
50 received physical therapy alone
53 received shockwave treatment
49 received prolotherapy (sugar water) injection
50 received PRP injection
Key Patient and Symptom Information:
Average patient age in study: 52 years old
Average symptom duration prior to treatment: 14-16 months
37.2% of patients were male while 62.8% were female
Key Results:
DASH (Disabilities of the Arm, Shoulder, and Hand) Score
Baseline (pre-treatment): No significant difference between any of the 4 studies groups
3 months: No significant difference between any of the 4 studies groups
6,18, and 24 months:
PRP: Patients showed statistically significant greater improvement than the physical therapy group
Prolotherapy: Patients showed statistically significant greater improvement than the physical therapy group
Shockwave: Patients showed no significant improvement compared to the physical therapy group
PRP versus prolotherapy
A separate analysis was performed comparing DASH scores for patients with greater than 12 months of symptoms
PRP group showed a statistically significant greater improvement in DASH scores than the prolotherapy group at 24 months post-treatment
SSS (Subjective Satisfaction Score) – Outcomes at 24 Months
PRP and prolotherapy: Statistically significant better patient satisfaction than physical therapy and shockwave
PRP versus prolotherapy: No significant difference in patient satisfaction
Key Take Home Points:
PRP and prolotherapy provided significantly better pain and functional outcomes than physical therapy and shockwave therapy at 6, 18, and 24 months after treatment.
PRP provided significantly greater pain and function improvement compared to prolotherapy for patients with greater than 12 months of symptoms.
Appointment:
Dr. Verma provides treatment for orthopaedic and sports medicine conditions of the shoulder, elbow, hand/wrist, hip, knee, and foot/ankle. If you are a patient interested in exploring treatment for your condition, please schedule a consultation with Dr. Verma to discuss the available options.
References:
Khan KM, Cook JL, Kannus P, et al. Time to abandon the ‘‘tendinitis’’ myth. BMJ. 2002;324(7338):626-627.
Kraushaar BS, Nirschl RP. Tendinosis of the elbow (tennis elbow): clinical features and findings of histological, immunohistochemical, and electron microscopy studies. J Bone Joint Surg Am. 1999;81(2):259-278.
Rees JD, Wilson AM, Wolman RL. Current concepts in the management of tendon disorders. Rheumatology (Oxford). 2006;45(5):508-521.
Shiri R, Viikari-Juntura E. Lateral and medial epicondylitis: role of occupational factors. Best Pract Res Clin Rheumatol. 2011 Feb;25(1):43-57.
Sanders TL, Maradit Kremers H, Bryan AJ, Ransom JE, Morrey BF. Health Care Utilization and Direct Medical Costs of Tennis Elbow: A Population-Based Study. Sports Health. 2016 Jul;8(4):355-8.
Puzzitiello RN, Patel BH, Forlenza EM, et al. Adverse Impact of Corticosteroids on Rotator Cuff Tendon Health and Repair: A Systematic Review of Basic Science Studies. Arthrosc Sports Med Rehabil. Apr 2020;2(2):e161-e169. doi:10.1016/j.asmr.2020.01.002
Lhee SH, Ryeol Lee K, Young Lee D. Comparing the Use of Physiotherapy, Shockwave Therapy, Prolotherapy, and Platelet-Rich Plasma for Chronic Lateral Epicondylosis: A Prospective, Randomized Controlled Trial With 2-Year Follow-up. Am J Sports Med. Published online August 15, 2025. doi:10.1177/03635465251361515